
By now you have probably heard about the injectible medications Ozempic, Saxenda, Wegovy, Zepbound and Mounjaro. Due to their effectiveness (and celebrity endorsement- good and bad)… they have created quite a buzz on the internet and social media!
Many of you may have been served ads for online clinics while scrolling through Instagram or gone done a rabbit hole on TikTok hearing all about “natural” equivalents that could “boost” your GLP-1 hormone. Oatzempic anyone?!....
There is a LOT of information out there, fact and fiction, when it comes to this “newer” medication drug class and as a board certified Internal Medicine and Obesity physician, I think it’s important to help you differentiate fact from fiction!
You may be wondering what to believe, how to sift through all the buzz, concerns about “Ozempic face” and who exactly should even be a candidate for treatment. Let’s discuss…
What are these medications?
These medications in the GLP-1 receptor agonist (GLP-1 RA) medication drug class are a powerful tool in our tool kit for treatment of diabetes and obesity and work in a unique way to address the root cause of many chronic cardio-metabolic diseases like type 2 diabetes, obstructive sleep apnea, and fatty liver disease, to name a few. In fact, Wegovy (semaglutide) got the FDA indication in 2024 for cardiovascular risk reduction on 20% in individuals with a history of stroke or heart attack who had overweight or obesity!
The first GLP-1 RA type medication, Byetta (exenatide) came out in 2009.
Initially approved for the treatment of type 2 diabetes, this drug class has evolved with different formulations, aiming for less frequent dosing, more impact on blood sugar control and now, 2 of them- Wegovy (semaglutide) & Zepbound (tirzepatide), are FDA-approved for the treatment of obesity.
They work through their action on GLP-1 receptors in the brain, gut and throughout the body resulting in altered gastrointestinal function, reduced appetite, effects on insulin function and body fat loss.
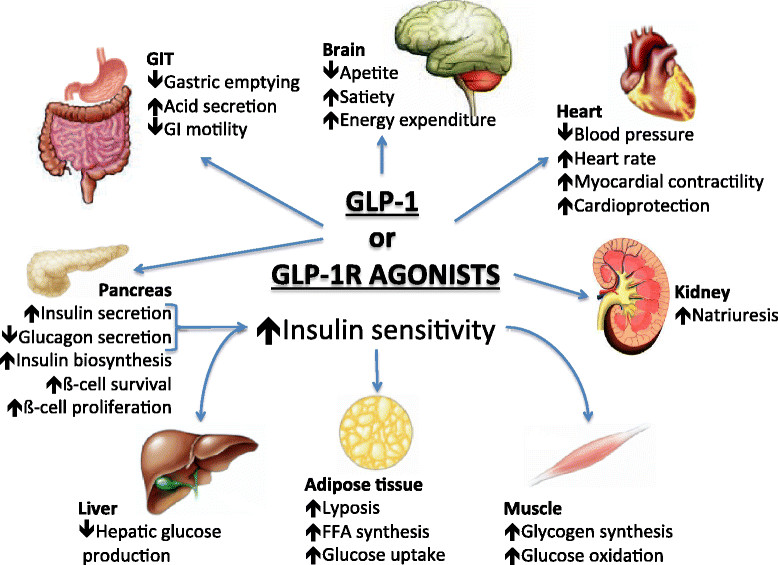
Illustration Credit: Saraiva, José & Sposito, Andrei. (2014). Cardiovascular effects of Glucagon-like peptide 1 (GLP-1) receptor agonists. Cardiovascular diabetology. 13. 142. 10.1186/s12933-014-0142-7.
Other Benefits!
In a recent study (August 2023), results were released by the manufacturer of Wegovy (Novo Nordisk) showing improvements in heart failure symptoms in those with congestive heart failure with preserved ejection fraction who were on Wegovy vs those who were not. Also in August 2023, results from another study showed Wegovy reduced the risk of heart attack, stroke or heart-related death in people with cardiovascular disease and obesity by 20% (no diabetes)!
These medications are revolutionizing the treatment and quality of life for people with congestive heart failure, type 2 diabetes and obesity and all its complications.
Along with many benefits, there do come potential medical risks. This is why it’s important to always weigh the benefits versus the risks of any medication and a topic I discuss with all of my patients.
Who is a Candidate for Using these medications?
Wegovy (semaglutide), Saxenda (liraglutide) and Zepbound (tirzepatide) are approved for the treatment of obesity for people with a BMI over 30 or a BMI > 27 with 1 weight-related condition.
Note on BMI, there are ranges by ethnicity, based on increased risk with high body fat, especially abdominal, at lower BMI ranges. Therefore, excess adiposity (especially visceral fat, not BMI) within the framework of personal history and medical history assessment is often a better way to assess risk.
Ozempic (semaglutide) and Mounjaro (tirzapetide) are approved for type 2 diabetes, and are used along with diet and lifestyle modifications.
Whether being used for type 2 diabetes or for weight management, special consideration should be made to use these medications (or any weight loss medication) appropriately and not in those who are underweight or those who have history of eating disorders and would be at risk.
Who needs medical supervision?
Anyone taking these medications… PERIOD.
It is not only important to screen for personal history of certain medical conditions, but also family history of conditions like medullary thyroid cancer, for which studies show lab rats had an increased risk.
There is a very real concern about muscle mass loss with any weight loss, especially when a significant amount is lost quickly. Also, any rapid weight loss can result in “Ozempic face”- not specific to the medication itself!
Muscle loss can occur if a person is not getting adequate nutrition, especially protein, is possibly on too high of a dose and/or not following weight training recommendations. Losing large amounts of muscle may seem like “good weight loss”, but the aim is to lose excess body fat, not just weight. This loss results in worsened overall cardio metabolic health.
In my practice, we follow muscle mass on body composition analysis monthly and monitor macronutrient intake, guide patients on resistance training and adjust dosing of medication to allow for adequate food intake. It is especially important to screen for nutritional deficiencies and manage these appropriately!
Along with muscle loss, another issue to look out for is avoiding dehydration as often thirst signals are not felt as much on these medications. Kidney function can be impacted by extreme dehydration, especially in the setting of extreme nausea and vomiting. It is important to avoid this type of situation as there are cases of kidney failure in individuals on these medications.
Last, your healthcare team should guide you in how to manage nausea and constipation, some common side effects, which you should not have to suffer through.
Not a Quick Fix
These medications are not to be used as a “quick fix” or “jumpstart”. If a person is considering only using them for a short period time, they will not get long term benefits and are at risk for weight regain!
For example, the STEP 4 study for Wegovy (semaglutide) showed weight regain in those individuals who stopped the medication at week 20 vs those who continued it and saw continued weight loss and then maintenance. In another extension trial, the group that stopped semaglutide regained 2/3 of the weight they had lost over a year, compared to those that stayed on semaglutide who maintained.
This kind of use of medication off and on can set a person up for cycles of weight loss and weight regain, which is risky not only medically, but psychologically.
When using any medication for diabetes management or for treatment of obesity, they are always used best along with lifestyle modifications!
For overall health outcomes and for the sustainability of the lifestyle change, I practice lifestyle medicine to help patients to establish a healthful dietary pattern, reduce intake of ultra-processed foods, explore and address eating behaviors, practice physical activity, get healthy amounts of sleep and practice healthy stress coping behaviors.
Use Caution
I can understand the temptation for those who may be struggling to get access and insurance coverage for these medications to use compounded formulations. These compounded peptides are NOT FDA-approved medications. The Obesity Medicine Association has issued a position statement regarding concerns that these peptides do not have the same safety, efficacy and purity of FDA-approved ones.
In such situations when a person would benefit from body fat loss and these medications are not feasible due to availability or cost, a physician trained in obesity medicine can offer alternative medication regimens that could be safe and effective. Alternatives like Qsymia, Contrave, metformin off label, and phentermine can be considered.
Lastly, if you are taking any medications for type 2 diabetes or for obesity treatment, ensure you are taking them with close medical supervision and while implementing healthful lifestyle changes. Often, diabetes and blood pressure regimens need to be adjusted as people require less of those medications!
Ensure your program and provider are using the right dose for you, taking into consideration your body composition and monitoring for muscle loss, guiding you in terms of healthy lifestyle changes and helping provide you with a plan for weight maintenance in the long term, whether on these medications, using alternative medications or without medications.
One way you can ensure a good plan of care is by working with a physician who has received training and is a Diplomate of the American Board of Obesity Medicine.
We are pleased to provide evidence-based diabetes and obesity care throughout Texas working with patients in-person and via telemedicine.
There are several new therapies on the horizon and it is an exciting time for medicine and the treatment of cardiometabolic disease. I will keep you updated!
In health,
Richa Mittal MD
